Arthritis

Arthritis is a complex joint disorder characterized by inflammation and the gradual deterioration of joint tissues. This deterioration often leads to a range of symptoms, including:
- Joint Pain: Persistent or intermittent discomfort in one or more joints, exacerbated by movement or pressure on the affected area.
- Joint Stiffness: Feeling of rigidity or limited flexibility in the joints, especially noticeable after periods of rest or in the morning.
- Joint Swelling: Visible or palpable enlargement of the joints due to swelling and inflammation.
- Redness and Warmth: Increased blood flow to inflamed joints may cause redness, warmth, or a sensation of heat.
- Decreased Range of Motion: Difficulty moving joints through their full range of motion, resulting in reduced flexibility and mobility.
- Fatigue: Persistent feelings of tiredness or lethargy, often associated with the body’s response to chronic pain and inflammation.
- Joint Deformity: Advanced cases of arthritis can lead to changes in joint shape and alignment, resulting in deformities.
- Systemic Symptoms: Certain types of arthritis, such as rheumatoid arthritis, may also present systemic symptoms like fever, weight loss, and overall malaise.
These symptoms can vary in intensity and may impact daily activities and overall quality of life. It’s important to schedule an appointment with your doctor if you feel you are experiencing any of these symptoms so you can be evaluated and receive appropriate diagnosis and treatment.
Early detection and management of arthritis symptoms can help prevent further joint damage and improve long-term outcomes. Your doctor can provide personalized guidance, recommend lifestyle changes, prescribe medications, or refer you to a specialist for further evaluation and care. Don’t delay seeking medical attention if you suspect you may have arthritis or are experiencing any related symptoms.
Arthritis can be caused by various factors, including:
- Age: Cartilage naturally wears down over time.
- Genetics: Some people may inherit a predisposition to arthritis.
- Obesity: Excess weight puts added stress on the joints, leading to accelerated cartilage breakdown.
- Injury: Trauma to a joint can increase the risk of developing arthritis in that joint.
- Autoimmune diseases: Conditions such as rheumatoid arthritis involve the immune system mistakenly attacking the joints.
While certain risk factors for arthritis, such as age and genetics, are beyond our control, there are steps you can take to reduce the risk or delay the onset of arthritis:
- Maintain a healthy weight to reduce stress on the joints.
- Engage in regular exercise to strengthen muscles and support joint function.
- Protect joints from injury during physical activities or sports.
- Eat a balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids.
- Avoid smoking, as it can contribute to the development of certain types of arthritis.
Arthritis is typically diagnosed through a combination of medical history, physical examination, imaging tests, and laboratory tests. The diagnostic process may involve the following:
- Medical History: Your doctor will review your medical history, including symptoms, their duration, and any factors that may contribute to arthritis, such as previous injuries, family history, or underlying health conditions.
- Physical Examination: A thorough physical examination will be conducted to assess joint function, range of motion, swelling, tenderness, and signs of inflammation.
- Imaging Tests: Imaging tests such as X-rays, magnetic resonance imaging (MRI), or ultrasound may be ordered to visualize the internal structures of the joints, detect any abnormalities in bone or cartilage, and assess the extent of joint damage.
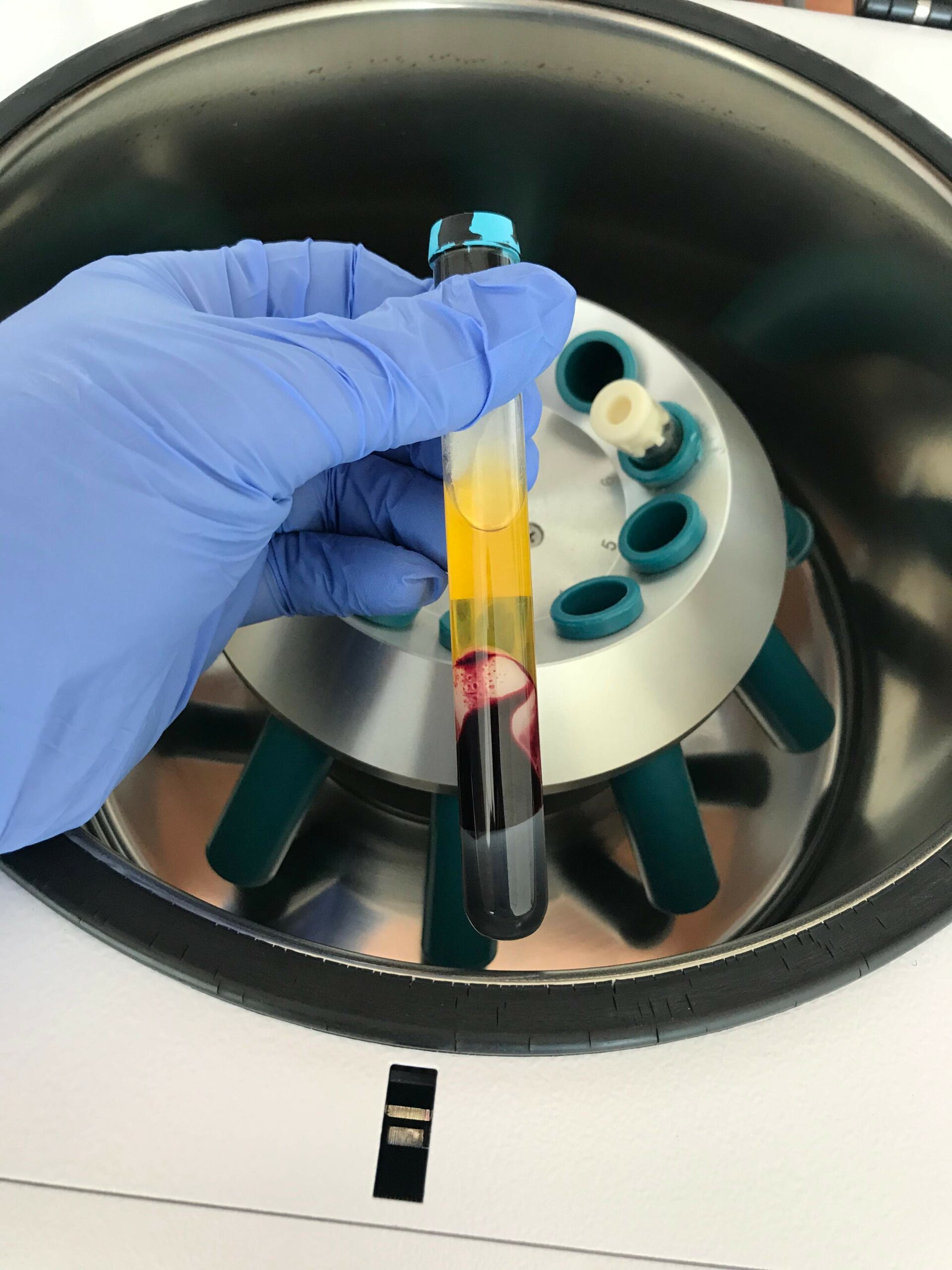
- Laboratory Tests: Blood tests may be performed to check for specific markers of inflammation or autoimmune activity, which can help differentiate between different types of arthritis.
- Joint Fluid Analysis: In some cases, a procedure called joint aspiration may be performed to remove a sample of fluid from the affected joint for analysis. This can help identify the presence of crystals (as seen in gout or pseudogout) or signs of infection.
Treatments for arthritis aim to manage symptoms, improve joint function, and slow disease progression. These options include:
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and disease-modifying antirheumatic drugs (DMARDs) may be prescribed to reduce pain and inflammation.
- Physical therapy: Exercises and stretches can help improve joint flexibility, strength, and mobility.
- Lifestyle modifications: Adaptations such as using assistive devices, maintaining proper posture, and avoiding repetitive movements can alleviate strain on affected joints.
- Injections: Corticosteroid or hyaluronic acid injections may be administered directly into the joint to provide relief.
- Surgery: In severe cases, joint replacement surgery may be recommended to replace damaged joints with artificial ones, restoring function and reducing pain.
At Anti-Aging Medical & Laser Clinic, we recognize the significant impact arthritis pain can have on daily life, hindering routine activities and diminishing overall well-being. That’s why our focus is on providing non-surgical solutions that efficiently alleviate pain and improve comfort.
At Anti-Aging Medical & Laser Clinic we offer cutting-edge injection treatments tailored to sports medicine and rehabilitation, including Prolotherapy, Platelet-Rich Plasma (PRP), SportVis (Hyaluronic Acid (HA)), and Cingal (Hyaluronic Acid + Cortisone) injections. However, before proceeding with these treatments, it’s crucial to undergo X-rays and potentially further imaging tests to accurately assess your condition and tailor a suitable treatment plan for you.